Blog Category: Healthcare
Agentic AI in Healthcare: Transforming Operations and Patient Experience

For as long as we can remember, healthcare has been an overburdened industry.
Patient influxes. Staff shortages. Rising operational costs – The challenges are numerous and continue to grow.
But there is hope for a smarter and more resilient future in healthcare, with Agentic AI.
While 80% of hospitals are already using some AI to enhance patient care and workflow efficiency, agentic AI takes a notch higher.
Let’s explore what agentic AI in healthcare means and where it can make a difference.
What is Agentic AI in Healthcare?
Agentic AI in healthcare refers to an artificial intelligence system that operates with a high degree of autonomy, adaptability, and decision-making ability, enabling it to perform healthcare workflows with minimal human intervention.
We know what you’re thinking: How is it really different from traditional AI already prevalent in healthcare?
There are two keywords here: autonomy and decision-making ability.
While traditional AI still follows predefined rules or models, agentic AI can perceive context, set goals, plan actions, and adjust based on real-time data and outcomes while ensuring compliance with medical bodies and patient safety. It goes further by moving from basic automation to goal-driven autonomy.
Consider this example for better clarity:
- Traditional AI: A chatbot that answers FAQs and schedules appointments using fixed scripts.
- Agentic AI: An autonomous agent reviews symptoms, analyzes medical documents, monitors test results, and alerts doctors in case of early signs of complications.
Agentic AI is powered by Large Language Models (LLMs) that can process vast amounts of data like clinical notes, patient histories, lab results, and medical guidelines to extract actionable insights.
Agentic AI Use-Cases in Healthcare
It’s no longer a question of whether agentic AI will reshape healthcare, but where it’s already doing so. Let’s explore real-world scenarios where agent-based systems are driving measurable improvements in patient care and enabling healthcare AI transformation.
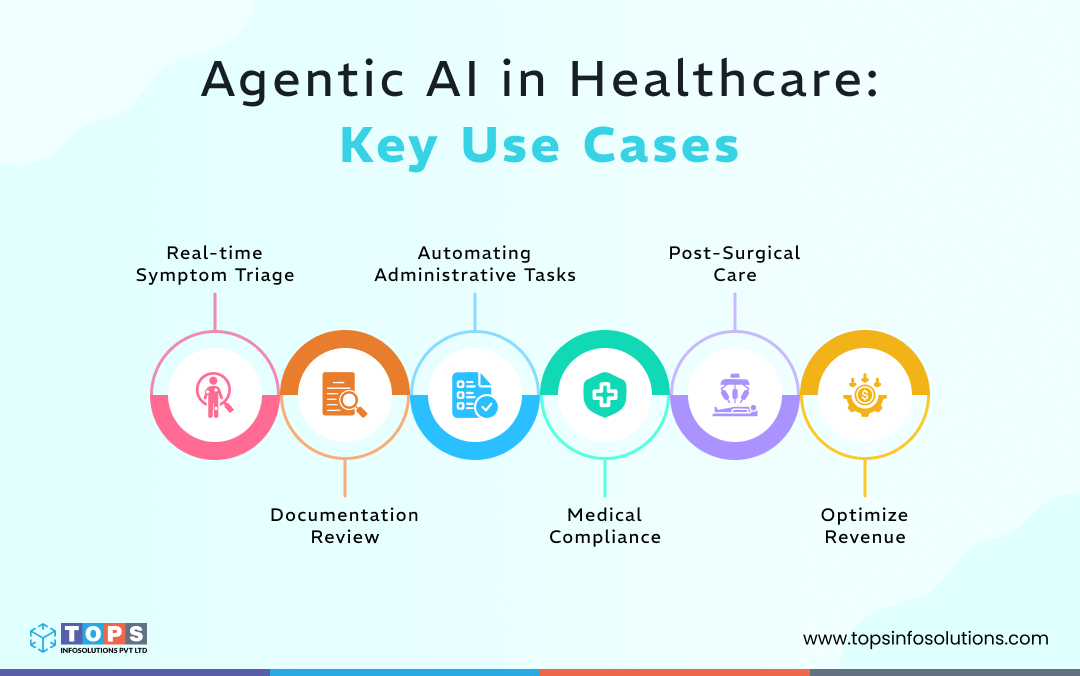
1. Real-time Symptom Triage
In healthcare, every second counts. But reality is far from it. Triage systems rely on manual assessments that delay determining the urgency of care.
Agentic AI changes that. An autonomous agent can assess symptoms, prioritize cases, and route patients to the right care level in real-time. Here’s how it works:
- Conversational assessment: The agent engages the patients, asks clarifying questions, and collects symptoms interactively.
- Context-driven decisions: It extracts patient data from its database, cross-references that with recent lab results or wearable devices to gauge severity.
- Instant escalation: It detects high-risk indicators like chest pain plus abnormal heart rate and immediately alerts an ER doctor while advising the patient to seek emergency care.
2. Documentation Review
When I say document review, I don’t just mean flipping through patient records. It’s a multi-layered process that involves:
- Verifying information against central records
- Professional evaluation of the patients, tests, and reports
- Assessing discharge summaries
It’s crucial to note that these are high-stakes tasks. One missed detail can impact care quality or compliance. Yet they eat up hours of a clinician’s day.
Here’s how agentic AI in healthcare helps:
-
Automated data extraction with OCR
With Optimal Character Recognition (OCR), agentic AI reads through medical documents, extracts key details, and validates them against the EHR (Electronic Health Records).
-
Intelligent clinical coding
AI agents assign and review clinical codes like SNOMED CT or ICD for consistency and flag errors. These codes also allow for accurate billing and insurance claims, regulatory compliance, and improved patient care.
Read More: Healthcare Documentation’s New Chapter: The Rise of Advanced Clinical Coding
-
Gap detection and clarification
AI agents can detect any missing information, like allergy details or incomplete diagnoses, and proactively ask for clarification before approval.
-
Summarized reports for quick decisions
After doing the documentation reviews, the agent generates a clean, structured summary so doctors can focus on decisions instead of drowning in paperwork.
3. Automating Administrative Tasks
Speaking of paperwork, isn’t it just never-ending in healthcare? From scheduling appointments to coordinating referrals, administrative tasks keep piling up. Unfortunately, they often pull focus away from patient care. This is where agentic AI shines. Some of the tasks it can automate are:
-
Schedule appointments
A scheduling AI agent checks doctor availability, matches it with patient preferences, and even manages last-minute cancellations, along with booking slots.
-
Automating referrals
When a patient seeks a specialist, the agent routes the case, sends reports, and ensures the appointment is confirmed.
-
Predicting supply chain needs
You can integrate the agentic AI into your supply chain systems, and it can determine what you’ll need to purchase next. From gloves to critical meds, the agent forecasts inventory based on usage patterns.
-
Onboarding a new patient
As soon as a new patient raises a query, the agent collects history and verifies documents from the central database and sets up the initial consultation without staff intervention.
-
Analyzing Patient Feedback
One important use case of agentic AI is collecting satisfaction scores, detecting patterns, and recommending process improvements.
4. Medical Compliance
The healthcare sector is loaded with a bunch of regulations, such as HIPAA and HITECH. Every patient record needs to be handled with top-notch security and accuracy. Failing to follow these compliances means dealing with penalties, lawsuits, and compromised patient trust.
Since manually adhering to them is time-consuming and, worse, error-prone, AI agents step in the following ways:
-
Real-time data monitoring
Traditional monitoring methods rely significantly on periodic audits, whereas AI agents can constantly scan data, transactions, and communication in case there’s a deviation from established policies or regulatory requirements.
-
Automated policy enforcement
The agent checks every healthcare workflow against regulatory bodies like HIPAA or GDPR. If any process violates policy, it halts it immediately and sends alerts.
-
Document compliance checks
Agents review clinical documents for mandatory fields, clinical coding standards, and completeness before submissions. It also flags missing consents and incorrect patient identifiers that are critical for compliance.
5. Post-Surgical Care
The patient experience doesn’t end with surgery and checkouts. There’s obviously recovery monitoring, tracking medications, and catching complications before they escalate. It’s challenging for clinicians to put up with it because of physical burnout and the sheer number of patients. With AI agents, healthcare facilities can provide:
-
Medication reminders
You can deploy reminder agents that notify patients to take their daily medications and even confirm adherence to reduce the cases of readmissions.
-
Care coordination
Agents can update patient EHR automatically and keep different healthcare personnel in the loop, improving coordination without back-to-back calls and messages.
-
Personalized recovery plans
Instead of following one-size-fits-all instructions, agentic AI can adjust care plans dynamically based on patient progress and feedback.
6. Optimize Revenue
Considering the workforce shortages and rising patient expectations, it is essential to make the revenue cycle a strategic priority for healthcare leaders seeking sustainable performance. Every manual task in the revenue cycle has a cost associated with it, be it denied insurance claims or delayed payments. To avoid these, AI agents can help with the following workflows:
-
Claims submission
AI agents gather and integrate billing data for accurate claims and ensure compliance by validating the claims against payer requirements. It also checks for errors and missing data, reducing delays.
-
Denial management
Agents can analyze denial data and highlight trends to provide actionable insights and corrective measures. It can predict which claims are likely to be denied based on historical patterns.
-
Revenue forecasts
AI agents can assess the current financial data along with patient history to provide accurate forecasts and revenue insights for better financial planning.
Ethical Impact of Agentic AI in Healthcare
One of the key differentiating factors of agentic AI is that it’s autonomous. But we need to consider the AI ethics in healthcare and question this autonomy. To what extent are healthcare AI agents allowed to make decisions? How do we address the AI bias, and who takes accountability for bad decisions – decisions that can have dangerous consequences?
Here’s the thing: healthcare environments are volatile, and autonomous decision-making is a double-edged sword. Humans, unlike AI, won’t make the same decisions for every case or patient. They’ll take into account the cultural factors and consider situational awareness backed by empathy before suggesting treatments. There’s a gap in values that won’t fill in anytime soon. Research suggests that 60% of healthcare organizations’ biggest challenges in using AI in patient care were the risk concerns and considerations.
To ensure agentic AI is used the way we want it to in healthcare, we need to consider the following ethical implications:
Decision-making transparency
To gain the trust of healthcare professionals, they must know how agents make decisions. Having a clear breakdown of the process helps in building confidence. For example, if an agent recommends switching a patient’s medication, it shows the reasoning: “Based on the patient’s recent lab results, allergy profile, and reaction history, this alternative reduces side-effect risks.”
Data privacy and security
AI agents get access to numerous personal records and sensitive information about the patients. While there are necessary compliance measures in place, there are still concerns about data breaches and unauthorized access. AI agents must ensure end-to-end encryption, role-based access control, and secure audit trails.
Bias and fairness
AI systems are no miracle. They’re just an intricate web of data. If it’s fed a specific set of data for a specific demographic, it can lead to unequal care recommendations based on gender, ethnicity, or socioeconomic background. Using diverse data sets and applying regular model audits is critical to maintaining equitable outcomes for all patients.
While there are multiple use cases for agentic AI in healthcare, healthcare professionals need to draw the line between low-stakes and high-stakes. Agents cannot take corrective actions, and there needs to be a human intervention after a certain point. An end-to-end automation is not just challenging but also inadvisable for the safety and well-being of patients.
Building Healthcare Agentic AI Systems the Right Way
As healthcare is evolving, it is only a matter of time before AI trends in healthcare evolve with it. As healthcare keeps patient care at the center of its operations, AI agents are the key to making that happen, be it through remote monitoring or faster response times. These agents take on the rudimentary tasks and do most of the heavy lifting so healthcare professionals can provide the best care for patients.
However, the future of agentic AI in healthcare needs to be accompanied by serious ethical responsibilities. Implementing agentic AI isn’t just about automation but about ensuring transparency, fairness, and security. Rushing into deployment without addressing bias, data privacy, and decision-making safeguards can do more harm than good.
To build AI agents that are secure, compliant, and trustworthy, you need to partner with a custom healthcare AI solutions provider who understands both the technology and the ethics behind it.
Revolutionizing Clinical Coding: A New Era in Healthcare Documentation

Healthcare involves multiple risk factors, one being handling the complexities of clinical documentation. The patient’s records and healthcare details are crucial to manage within the clinical space. They are further used for multiple pivotal processes including billing, reimbursements, insurance, healthcare policies & planning, and analysis of epidemiological areas.
Clinical coding converts patient records into encoded reports following a structured and unified coding system. Manually coding clinical data is a non-trivial and time-consuming task with high susceptibility to human errors.
As these further impact the other healthcare processes, even the slightest mistake in the process can lead to big blunders and far-reaching consequences. Clinical code assignment simplifies the complex and voluminous clinical records into standard clinical documentation.
“Clinical code is the unified foundation of storing, retrieving, and maintaining healthcare documentation.”
What is Clinical Coding and Why is It Crucial?
The process of clinical coding is a systematic process of deciphering the medical diagnosis, procedures, and clinical information into standardized codes. The assigned clinical codes are derived from the global coding system such as SNOMED CT (Systematized Nomenclature of Medicine-Clinical Terms), ICD, CPT, etc. These codes are assigned to ensure that the overall global health data records are processed, stored, and shared in a consistently structured format.
As per a report by Healthcare Finance, improper clinical coding costs the US healthcare system around $262 Billion annually.
This process allows for:
- Accurate billing and insurance claims
- Improved patient care approach
- Regulatory compliances
Though this process simplifies healthcare documentation to a great extent but also imposes a set of challenges that hinder the efficiency and accuracy of the healthcare ecosystem.
Present Challenges in the Clinical Coding
As we have already discussed above, clinical coding comes with a set of challenges. Even the expert coders with years of experience in the domain get stuck to fetch the right codes balancing accuracy and productivity at the same time.
Converting clinical documents into numeric codes or ConceptIDs is fundamentally important to follow a standard approach for recording or sharing clinical data globally. The challenges of clinical coding affect the overall operational and financial efficiency of healthcare organizations and hence, need to be addressed in some way.
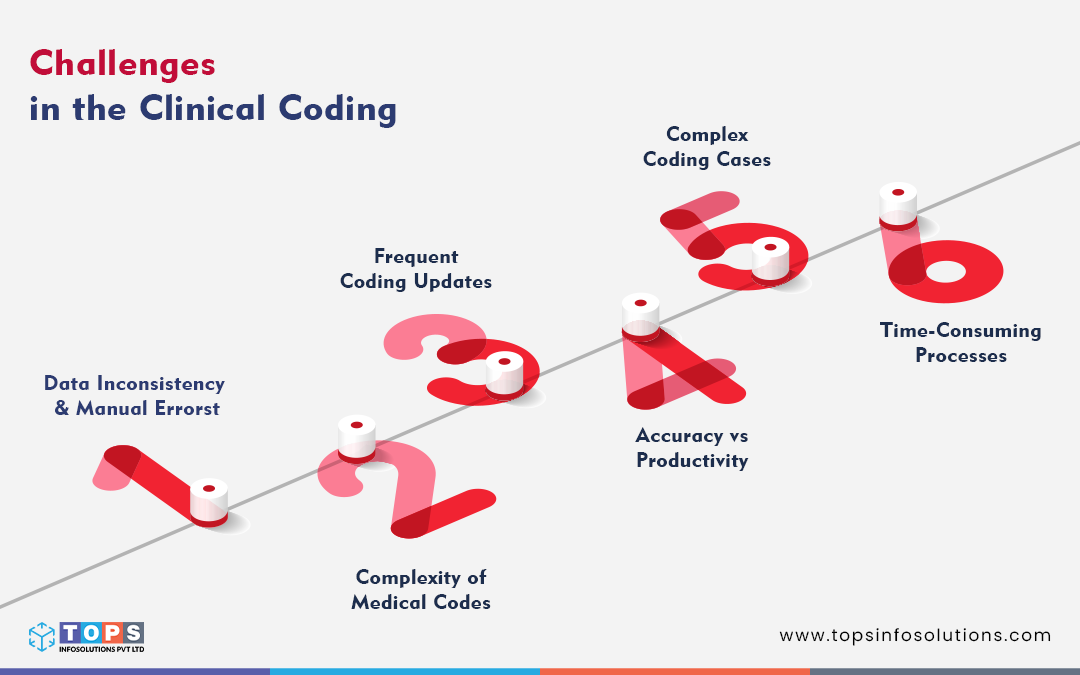
Data Inconsistency & Manual Errors
The complexities of the clinical documents and complete reliance on human input are the best combination to bring about the chances of errors in code assignment and documentation management.
Considering the vast ecosystem of healthcare including multiple diseases, diagnoses, drug formulations, common symptoms, etc, understanding the clinical report accurately and assigning the right codes accordingly is challenging.
The chances of misinterpretations, typing errors, and mistakes in codes can cause data inconsistency, incorrect diagnosis, billing issues and affect patient care.
Complexity of Medical Codes
Millions of clinical codes are available with thousands of millions of code combinations possible. Assigning the exact and most accurate code as per the disease symptoms and diagnosis is as crucial as challenging.
Moreover, any inaccuracy in the process may further lead to incorrect reports, delayed billing processes and reimbursements, and false or inaccurate insurance claims.
Frequent Coding Updates
The coding standards for clinical codes are frequently updated. Any new symptom or disease identification, drug inventions, new diagnosis discoveries, etc causes changes in the coding ecosystem.
Clinical coders need simultaneous education or training for the updates for easy adaptation and maintaining accuracy.
Accuracy vs Productivity
Achieving accuracy as well as productivity in the clinical coding process is not a practical approach. While accuracy is essential for further operations like billing, or reimbursement, focusing solely on accuracy may hamper productivity to a great extent.
Complex Coding Cases
Sometimes clinicians or clinical coders encounter highly complex patient reports with no exact code matching. In such scenarios, they need to create the most matched clinical code combinations to represent the case complexity.
Time-Consuming Processes
Clinical coding is a slow and labor-intensive process, where clinical coders need to sift through lengthy clinical records to extract the required detail and match it to the right codes.
There are many more challenges that healthcare regulation authorities face due to inaccuracy in clinical coding like data processing delays, interdisciplinary communication, and more.
Simplifying Clinical Coding for Better Accuracy
The importance of clinical coding within the healthcare sector is indisputable as it affects overall operational efficiency. Technological advancements simplify the overlong and complex clinical coding process to a great extent. With technologies like AI, NLP, ML, and cloud-based platforms, clinical coders can address the inherent challenges of manual coding and reduce the chances of errors.
Automating the entire clinical coding is not the right approach as it anyway needs human intervention for either code verification or managing the flow of AI operations. But with the help of these technologies or clinical coding tools, the chances of manual errors, and inaccuracies across data, can be avoided while achieving time efficiency in the process.
Benefits of Automated Clinical Coding:
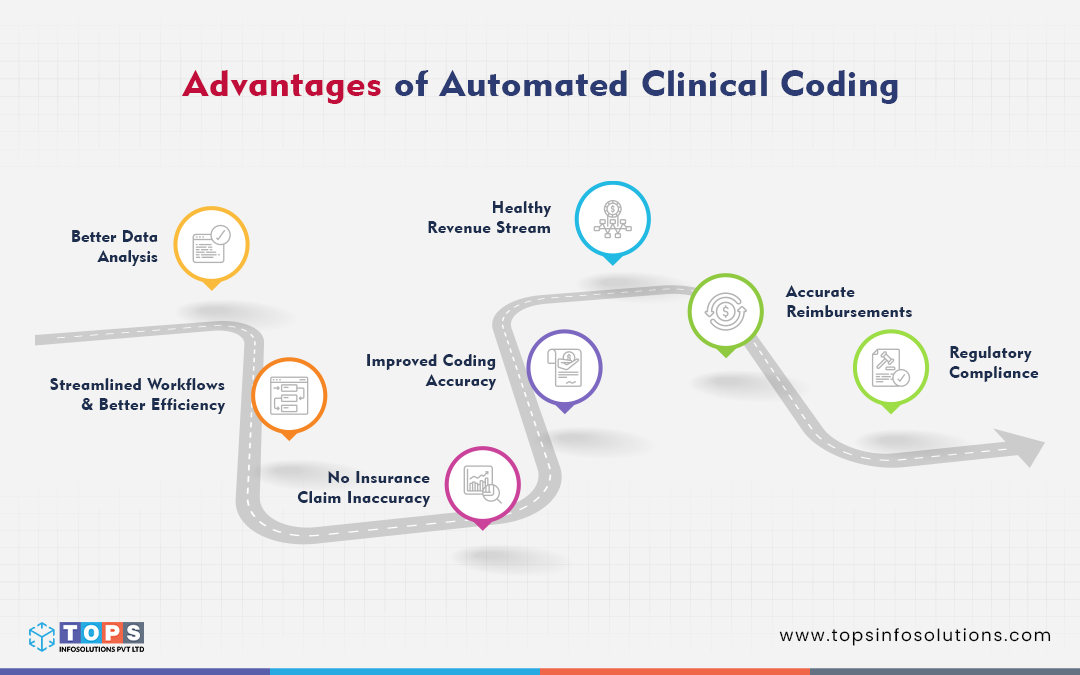
Improved Coding Accuracy
Maintain a high level of accuracy with clinical documents while avoiding manual errors in the clinical coding process.
Streamlined Workflows & Better Efficiency
Automated AI clinical coding helps clinical coders with an efficient and more streamlined coding approach.
Better Data Analysis
Analyse and process the medical report documents without missing any details for accurate clinical coding.
No Insurance Claim Inaccuracy
Any discrepancy in medical reports may lead to false or erroneous insurance claims, but with automation in clinical coding, insurance claims inaccuracy can be avoided to a great extent.
Healthy Revenue Stream
Speedy claim submissions, accurate medical billing, and reimbursement processes reduce the load of RCM staff and help create a better and healthier revenue cycle.
Accurate Reimbursements
Automating the process of clinical coding with correct medical codes, and low human errors results in faster claim processing and reduced denial rates to ensure accurate reimbursement.
Regulatory Compliance
Real-time auditing and minimized coding errors enhanced regulatory compliance adherence, avoiding claim denials and penalties due to non-adherence to the coding guidelines.
Docs4Docs: Bringing Down the Clinical Code Complexities
Docs4Docs is developed as a web-based platform to allow clinicians and health organizations to generate, manage, and share high-quality clinical documents. With the incorporation of advanced technologies, Docs4Docs automates the entire clinical documentation process with faster and more accurate clinical coding experience.
While developing Docs4Docs for our client, we struggled with building a function to fetch the right codes from the millions of available codes and maintain the accuracy level of clinical documents while balancing productivity. But with consistent brainstorming, strategic minds, and great coding skills, e have implemented various methodologies like custom AI logic, training AI with cross co-relations, vector database, etc.
How Docs4Docs works for clinicians:
Automated Code Assignment
After the document upload, Docs4Docs automatically converts the text report into image form to scan the clinical records, extract the medical terms, and assign relevant SNOMED CT codes.
Modification/Edit Window
Coders can check if the text extraction is correct or not to avoid any inaccuracy in the clinical codes.
Time-Efficient Clinical Coding
With real-time data processing and monitoring of medical data, Docs4Docs accelerates decision-making, and workflow efficiency and helps with administrative workload.
Human-in-Loop Approach
Even AI alone cannot handle the complexities of clinical coding, hence the expert clinical coder does the final verification of the assigned clinical codes to allow AI to generate the final report. Any changes in the codes can be made before report generation.
No doubt clinical coding is the cornerstone for effective and systematic clinical documentation. Everything works over data and for the healthcare industry, efficiently recording, processing, and sharing patient information is the utmost priority. Any kind of disparity in the data further affects the various processes including insurance claims, billing, reimbursements, fetching patient medical history, and more.